Understanding Degenerative Disc Disease: A Closer Look at Its Stages
Degenerative disc disease (DDD) is a common condition affecting the spine, primarily characterized by the gradual deterioration of the spinal discs. While the decline can be attributed to aging, it doesn't always result in pain or significant symptoms for everyone. Understanding the stages of this condition is vital for anyone experiencing discomfort, as early intervention can significantly improve outcomes.
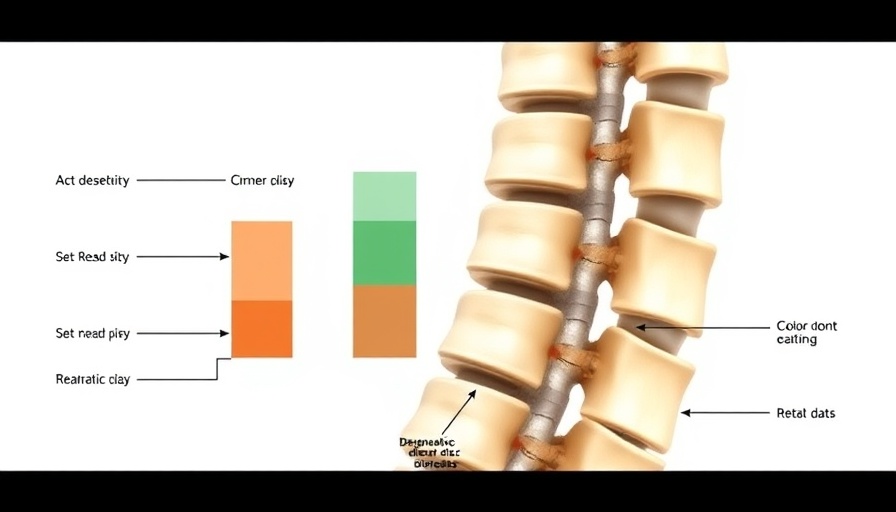
The Four Stages of Degenerative Disc Disease
DDD progresses in four distinct stages, each presenting different symptoms and challenges.
Stage 1: Subtle Beginnings
In the initial stage, most individuals may remain symptom-free. However, slight changes such as a loss of spinal curvature hint at the onset of degeneration. Addressing even these minor indicators early can prevent further strain and deterioration.
Stage 2: The First Signs of Pain
As the disease evolves, symptoms become more pronounced. Disc thinning and the formation of bone spurs can lead to noticeable discomfort. A narrowing spinal canal can also trigger pain, compelling many to seek treatment.
Stage 3: Major Changes and Increased Pain
At this stage, postural changes become evident, and pain can become chronic. Limited mobility and nerve damage might occur as the discs continue to degenerate and scar tissue forms. This stage is crucial; intervention can help alleviate pain and maintain mobility.
Stage 4: Advanced Degeneration
The final stage often symbolizes irreversible damage, with severely thin or even absent discs. This can lead to substantial pain and rigid spinal structures. In severe cases, bones may fuse, leading to other complications.
How Chiropractic Care Can Aid You
Chiropractic care offers a safe, non-invasive way to handle degenerative disc disease. Regular adjustments can restore spinal alignment, while therapies such as spinal decompression promote healing by alleviating nerve pressure. These methods not only relieve pain but can also help slow the progression of DDD.
Take Action Today
The key to managing degenerative disc disease lies in early action. By seeking chiropractic care sooner rather than later, you can effectively manage symptoms and enhance your quality of life. Reach out to a chiropractic provider to explore treatment options that can lead you on the path to a healthier, pain-free existence.
 Add Row
Add Row  Add
Add 




Write A Comment